Welcome To The Healthy Indiana Plan
The Healthy Indiana Plan is a health-insurance program for qualified adults. The plan is offered by the State of Indiana. It pays for medical costs for members and could even provide vision and dental coverage. It also rewards members for taking better care of their health. The plan covers Hoosiers ages 19 to 64 who meet specific income levels. See below if your 2022 income qualifies.
- Individuals with annual incomes up to $18,764 may qualify.
- Couples with annual incomes up to $25,276 may qualify.
- A family of four with an annual income of $38,300 may qualify.
The Healthy Indiana Plan uses a proven, consumer-driven approach that was pioneered in Indiana. The program continues to build upon the framework and successes of the original Healthy Indiana Plan that started in 2008.
If you have any questions, or to find out if you may be eligible to participate in the Healthy Indiana Plan, please consult the menu on the left of this page, or contact 877-GET-HIP9 .
What If I Quit Or Lose My Job
In most cases, when you quit or lose your job, you also lose your job-based health insurance coverage.
You might be eligible to temporarily continue your coverage with COBRA or state continuation.
However, you have to be able to pay both your share of the premium and the part your employer had been paying.
Keep Your Information Up To Date
The federal Public Health Emergency will be ending soon. If you have an AHCCCS Medical Assistance/MA case, keep your information up to date so you can receive the latest information. Learn more about how AHCCCS is planning for the end of the Public Health Emergency.
To update your information, you may go online to . If you have any questions, you may call 1-855-432-7587, Monday through Friday 7:00 a.m. – 6:00 p.m.
The Arizona Health Care Cost Containment System is Arizona’s Medicaid agency that offers health care programs to serve Arizona residents. AHCCCS provides medical insurance coverage to thousands of Arizonans each year, for which DES provides eligibility services.
Health insurance through AHCCCS helps individuals cover the cost of doctors office visits, physical exams, immunizations, prenatal care, hospital care and prescriptions they need.
You May Like: Free Government Cell Phones For Seniors
Colorado Indigent Care Program
The Colorado Indigent Care Program provides discounted health care services to low income people and families. CICP is not a health insurance program. Services vary by providers.
Who Qualifies?
- You must be 18 and older
- You must be at or below 250% of the Federal Poverty Level
- You must be lawfully present in the United States and a legal resident of Colorado
- You cannot be eligible for Health First Colorado or Child Health Plan Plus
Top Benefits:
- Discounted health care services provided by participating Colorado hospitals and clinics
- No premium costs
- You are allowed to have primary health insurance or have Medicare
- CICP ratings are good for a full year, see program information page for exceptions
Co-pay Costs:
| Program Information Page |
Accessing Ohip Funded Physiotherapy
Many pt Health clinics across Ontario offer government funded physiotherapy services.
If you meet the eligibility criteria, and have a referral, find and contact a pt Health clinic near you. Please note that your referral may only be used at one clinic.
An Ontario health care is required for OHIP covered physiotherapy, unless you are approved for Ontario Disability Support or Ontario Works .
Don’t Miss: Government Programs To Help Remodel Home
Elderly Blind And Disabled Waiver
Waiver For Persons Who Are Elderly, Blind, or Disabled is a program to provide an alternative to nursing facility care for elderly, blind, or physically disabled persons.
Who Qualifies?
In order to be enrolled in EBD you must:
- either be 65 years of age and older with a functional impairment,
- or be between the ages of 18 and 64 and be blind or physically disabled
- be currently residing in, or be at risk of being institutionalized in a nursing facility or hospital
- have an income less than 300% the Supplemental Security Income allowance per month
- have countable resources less than $2000 for a single person or $3000 for a couple.
Top 5 Benefits:
- Adult day services
| Program Information Page |
How Health Insurance Helps
Health insurance protects you before you get hurt or sick.
If you get hurt or sick and need to go to the doctor, health insurance protects you from paying high medical bills.
Health insurance is also called a health benefit plan. Health benefit plans cover preventative services like wellness visits, shots, and screening tests. These services help you stay healthy and avoid future health problems.
Read Also: Definition Of Socialism In Government
Medicaid Covers A Broad Range Of Health And Long
Medicaid covers a broad range of services to address the diverse needs of the populations it serves . In addition to covering the services required by federal Medicaid law, many states elect to cover optional services such as prescription drugs, physical therapy, eyeglasses, and dental care. Coverage for Medicaid expansion adults contains the ACAs ten essential health benefits which include preventive services and expanded mental health and substance use treatment services. Medicaid plays an important role in addressing the opioid epidemic and more broadly in connecting Medicaid beneficiaries to behavioral health services. Medicaid provides comprehensive benefits for children, known as Early Periodic Screening Diagnosis and Treatment services. EPSDT is especially important for children with disabilities because private insurance is often inadequate to meet their needs. Unlike commercial health insurance and Medicare, Medicaid also covers long-term care including both nursing home care and many home and community-based long-term services and supports. More than half of all Medicaid spending for long-term care is now for services provided in the home or community that enable seniors and people with disabilities to live independently rather than in institutions.
Figure 5: Medicaids benefits reflect the needs of the population it serves.
What If I Lose My Job Outside Of Open Enrollment Open
The yearly period in the fall when people can enroll in a health insurance plan for the next calendar year. Open Enrollment for 2023 runs from November 1 through January 15, 2023. Enroll by December 15 for coverage that starts January 1.
In 2023, a job-based health plan is considered “affordable” if your share of the monthly premium in the lowest-cost plan offered by the employer is less than 9.12% of your household income.
A standard of minimum coverage that applies to job-based health plans. If your employerâs plan meets this standard and is considered âaffordable,â you wonât qualify for a premium tax credit if you buy a Marketplace insurance plan instead.
Also Check: How To Get Government Grant Money
Search For Financial Assistance From The Government
Benefits.gov is a free website that can help you determine which types of government assistance you might qualify for. You can also find out how and where to apply.
- Using the Benefit Finder, answer questions about yourself and your needs. Afterwards, you can find out if youre eligible for programs to help you pay for:
- Utilities and other necessities
Check back with Benefits.gov in the future to see if youre eligible for additional benefits. You can report major life events or see if new benefit programs have become available.
Applying For Apple Health Coverage
You have many options to apply for Apple Health coverage. Visit our Apply for or renew coverage webpage to learn more.
When youre ready to apply, youll need:
- Your household monthly income.
- The Social Security numbers and dates of birth for each member of your household.
- Your immigration information, if that applies to you.
Read Also: Assurance Wireless Free Government Phone
Can Immigrants Qualify
Medicaid is generally only available to immigrants if they’ve been legally residing in the U.S. for five years or more.
But lawfully-present immigrants can qualify for premium subsidies in the marketplace/exchange even if their income is below the poverty level. This ensures that low-income immigrants can still obtain affordable coverage while they wait five years to qualify for Medicaid.
Medicaid is not usually available to undocumented immigrants, but there can be exceptions. One example is short-term limited Medicaid coverage in an emergency or emergency coverage for people who are pregnant.
Again, Medicaid eligibility varies from state to state. For example, California has chosen to extend Medicaid eligibility to undocumented children and young adults who otherwise meet the income criteria for eligibility.
How To Get Coverage
You may have to wait until the next open enrollment period with your parents health plan to be added to their health insurance coverage.
However, if youve recently lost other comprehensive health insurance coverage, you might be able to enroll before open enrollment if you meet the health plans requirements for a special enrollment period.
You May Like: Government Programs To Start A Business
Who Pays For Medicaid
Medicaid is paid for by federal and state taxes. It is administered at the state level. That’s why coverage and eligibility rules vary from one state to another.
If you receive Medicaid, your friends, neighbors, and fellow citizens are paying for your health care with their tax dollars.
If you get Medicaid, youll likely be cared for at the same hospitals and by the same physicians as people who have private health insurance.
Even though Medicaid is government health insurance, most of the care provided to people who receive it comes from private businesses and healthcare providers. Most states contract with private insurance companies to administer coverage. On your ID card, you might the name and logo of a well-known insurance provider.
You can apply for Medicaid through your state’s ACA health insurance exchange or by contacting your states Medicaid program directly.
Ways To Apply For Chip:
- Fill out an application through the Health Insurance Marketplace®. If it looks like anyone in your household qualifies for Medicaid or CHIP, well send your information to your state agency. Theyll contact you about enrollment. When you submit your Marketplace application, youll also find out if you qualify for an individual insurance plan with savings based on your income instead. Create an account or log in to an existing account to get started.
FYI: Apply any time
You can apply for and enroll in Medicaid or CHIP any time of year. Theres no limited enrollment period for either Medicaid or CHIP. If you qualify, your coverage can start immediately.
You May Like: Car Insurance For Federal Government Employees
Health Insurance For Low Income
Everyone needs health care, but not everyone can afford health insurance. Learn about your options for coverage with low income.
Health insurance premiums are too expensive for some individuals and families. But going without health insurance is risky. If you were to face an unexpected illness or injury, the medical bills could be overwhelming, especially if you need ongoing care.
Medicaid Facilitates Access To Care
A large body of research shows that Medicaid beneficiaries have far better access to care than the uninsured and are less likely to postpone or go without needed care due to cost. Moreover, rates of access to care and satisfaction with care among Medicaid enrollees are comparable to rates for people with private insurance . Medicaid coverage of low-income pregnant women and children has contributed to dramatic in the U.S. A growing body of research indicates that Medicaid eligibility during childhood is associated with reduced teen mortality, improved long-run educational attainment, reduced disability, and lower rates of hospitalization and emergency department visits in later life. Benefits also include second-order fiscal effects such as increased tax collections due to higher earnings in adulthood. Research findings show that state Medicaid expansions to adults are associated with increased access to care, improved self-reported health, and reduced mortality among adults.
Figure 7: Nationally, Medicaid is comparable to private insurance for access to care the uninsured fare far less well.
Don’t Miss: Which Government Agency Is Responsible For Cyber Security
How Much Does Medicaid Cost How Is It Financed
Together, states and the federal government spent about $630 billion on Medicaid services in fiscal year 2018. State policies have a substantial impact on the amount the federal government spends on Medicaid, not only because states are guaranteed federal Medicaid matching funds for the costs of covered services furnished to eligible individuals, but also because states have broad discretion to determine who is eligible, what services they will cover, and what they will pay for covered services, as discussed above.
It costs Medicaid substantially less than private insurance to cover people of similar health status due primarily to Medicaids lower payment rates to providers and lower administrative costs.
The federal government contributes at least $1 in matching funds for every $1 a state spends on Medicaid. The fixed percentage the federal government pays, known as the FMAP, varies by state, with poorer states receiving larger amounts for each dollar they spend than wealthier states. In the poorest states, the federal government pays 73 percent of Medicaid service costs the national average is between 57 and 60 percent. As noted above, the federal government pays an enhanced 90 percent of service costs on a permanent basis for low-income adults covered by the ACA Medicaid expansion.
How Much Supplementary Health Or Dental Insurance Do You Need
There are a wide variety of supplementary health and dental insurance plans, each with their own level of coverage, but the amount of health insurance you need is a highly personal decision. Only you can decide how much is right for you, but an insurance agent or company may be able to help you make those decisions. Visit the finding an insurance agent or company section of Working With an Insurance Agent or Company to find someone who can help you.
Factors to consider when deciding how much coverage you need include:
- How much can you afford to pay each month? Each year?
- Do you have any other supplementary health insurance through your employer, a parents group plan or a spouse/partner?
- Do you require prescription drugs on an ongoing basis?
- Are you willing to share a hospital room, or do you prefer a private room?
- Do you wear glasses or contact lenses?
- Do you receive medical services from professionals such as chiropractors or massage therapists?
- Can you afford to pay out of pocket for ambulance fees?
- Do you have a chronic illness that requires more extensive medical services than OHIP provides?
- Do you have a pre-existing medical condition? Some supplementary health insurance plans do not cover this. Be sure to shop around to find an insurer who might.
Supplementary Health and Dental Insurance | 101: Getting Started 4
You May Like: How To Add Minutes To Safelink Government Phone
Ontario Community Physiotherapy Program
Are you seeking physiotherapy services for a youth or senior, or are you recovering from an illness, surgery or injury that required an overnight admission in the hospital, or receiving ODSP or Ontario Works?
You may be eligible for government funded physiotherapy services. Many of our clinics are authorized to offer these services and can work with you to get back your mobility and function.
Health Choice For Children
The North Carolina Health Choice Health Insurance Program for Children is a comprehensive health coverage program for low-income children. If you do not qualify for Medicaid, but cannot to afford private or employer-sponsored health insurance, your children may qualify for NC Health Choice.
Side Nav
Also Check: Free Internet With Government Assistance
Who Is Eligible For Medicaid
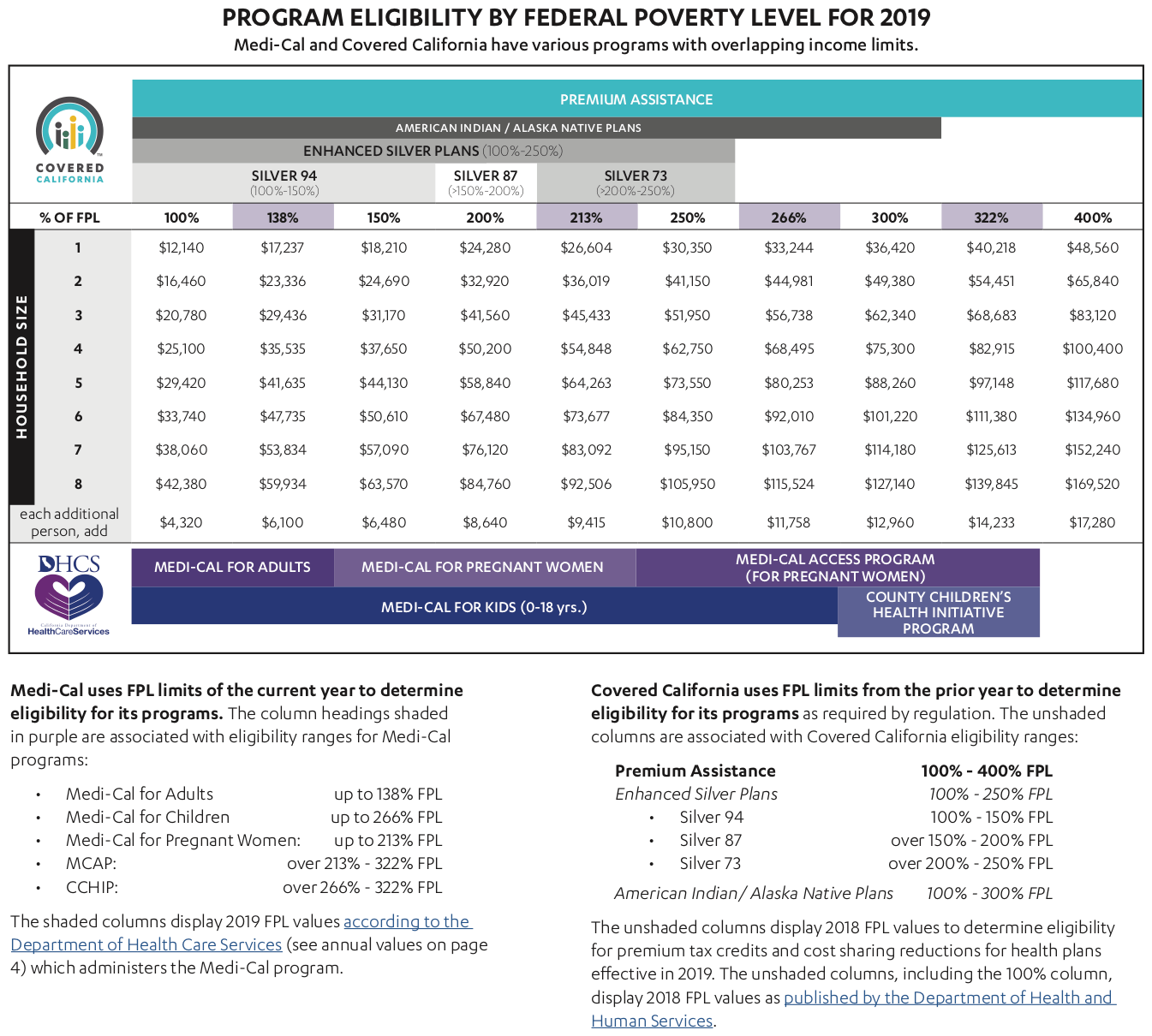
You may qualify for free or low-cost care through Medicaid based on income and family size.
In all states, Medicaid provides health coverage for some low-income people, families and children, pregnant women, the elderly, and people with disabilities. In some states the program covers all low-income adults below a certain income level.
- First, find out if your state is expanding Medicaid and learn what that means for you.
- If your state is expanding Medicaid, use this chart to see what you may qualify for based on your income and family size.
Even if you were told you didn’t qualify for Medicaid in the past, you may qualify under the new rules. You can see if you qualify for Medicaid 2 ways:
- Visit your state’s Medicaid website. Use the drop-down menu at the top of this page to pick your state. You can apply right now and find out if you qualify. If you qualify, coverage can begin immediately.
- Fill out an application in the Health Insurance Marketplace. When you finish the application, we’ll tell you which programs you and your family qualify for. If it looks like anyone is eligible for Medicaid and/or CHIP, we’ll let the state agency know so you can enroll.
Medicaid Coverage Has Evolved Over Time
Under the original 1965 Medicaid law, Medicaid eligibility was tied to cash assistance or federal Supplemental Security Income starting in 1972) for parents, children and the poor aged, blind and people with disabilites. States could opt to provide coverage at income levels above cash assistance. Over time, Congress expanded federal minimum requirements and provided new coverage options for states especially for children, pregnant women, and people with disabilities. Congress also required Medicaid to help pay for premiums and cost-sharing for low-income Medicare beneficiaries and allowed states to offer an option to buy-in to Medicaid for working individuals with disabilities. Other coverage milestones included severing the link between Medicaid eligibility and welfare in 1996 and enacting the Childrens Health Insurance Program in 1997 to cover low-income children above the cut-off for Medicaid with an enhanced federal match rate. Following these policy changes, for the first time states conducted outreach campaigns and simplified enrollment procedures to enroll eligible children in both Medicaid and CHIP. Expansions in Medicaid coverage of children marked the beginning of later reforms that recast Medicaid as an income-based health coverage program.
Figure 3: Medicaid has evolved over time to meet changing needs.
Recommended Reading: Government Grants For Hair Salons